Targeting a specific DNA-repairing protein in the brain could be an effective way to treat the most aggressive type of brain tumour, a study suggests.
Researchers at the University of Leeds found that inhibiting this protein, called RAD51, helped increase the effectiveness of radiotherapy in killing off glioblastoma cells in the lab.
Glioblastoma is the most common type of primary brain tumour in adults and also the most aggressive. Many patients will not survive the disease despite intensive treatment.
It is thought a subgroup of glioblastoma cells are able to reproduce to make identical copies of themselves and are more resistant to treatment.
In the new study, the researchers found that this subgroup of cells, called Glioblastoma Stem Cells (GSCs), have a large amount of the RAD51 inside them.
Professor Susan Short, Professor of Clinical Oncology and Neuro-Oncology in the School of Medicine and lead author of the study, said: “Radiotherapy damages the DNA in the glioblastoma cells – but the RAD51 helps them to repair this damaged DNA, meaning they can repopulate the tumour.
“By targeting RAD51 with an inhibitor we were able to make these GSCs more sensitive to the effects of radiotherapy, helping remove the tumour.
“The exact mechanism by which RAD51 becomes increased in cells that survive radiotherapy is not yet known but our study provides strong evidence that this is the right protein to target in the treatment of this aggressive brain cancer.”
The researchers, whose study is published in the journal Stem Cell Reports, used brain tumour cells taken from patients.
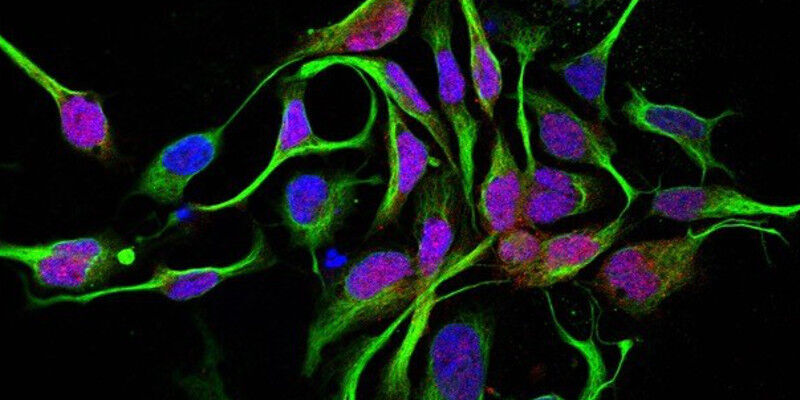
They used immunofluorescence microscopy to show that the glioblastoma cells have higher amounts of RAD51 than other normal brain cells.
They then combined an inhibitor agent with radiation to target the cells.
“The next step will be to find an inhibitor agent that can be used on humans,” said Professor Short.
“The inhibitors that we used are not yet suitable for clinical trials, but these results suggest that using equivalent agents or new drugs that target this same pathway will be important to investigate.”
The study was funded by Cancer Research UK.
Dr Justine Alford, Cancer Research UK’s senior science information officer, said: “Survival for glioblastoma is low and has seen little improvement over the years, so we urgently need better, kinder treatments for the disease.
“This promising study in cells and mice may have found a way to cut off the tumour’s fuel supply, which could one day help treatments target the disease more precisely and effectively. But more research is needed to find out if this strategy could be safe and effective in people.”
Glioblastoma primarily affects adults aged between 45 and 75 and is slightly more common in men than in women.
The average survival time is 12 -18 months. Only 20% of patients survive more than one year, and only 3% of patients survive more than three years.
Further information
Journalists can contact Sophie Freeman in the University of Leeds press office on 0113 343 8059 or email s.j.freeman@leeds.ac.uk
The image shows patient-derived glioblastoma cells.