Gene editing has been used to fix broken retinal cells in a laboratory setting.
Researchers hope it will pave the way for a treatment for the most common form of inherited blindness.
The discovery was made possible by a breakthrough in understanding the genetic mutations which cause retinitis pigmentosa.
The researchers, from the Universities of Leeds and Newcastle, found that mistakes in "proofreading" the genetic code of retinal cells cause mutations which lead to the disease.
Scientists studied the disease by creating a "retina in a dish" using stem cells derived from skin samples donated by patients at Leeds Teaching Hospitals Trust.
This new understanding of the disease process, published today in Nature Communications, is leading to the development of a gene therapy for retinitis pigmentosa.
The research team are now starting the next phase of this project and hope to embark on clinical trials with a gene therapy technique in the near future.
Co-author Professor Colin Johnson, from the Leeds Institute of Biomedical and Clinical Sciences, said: "We've been puzzled by the genetics behind these unique forms of inherited blindness for over 20 years.
"Our study is the first to really make sense of how these conditions develop, and I'm now very hopeful that this will lead to clinical trials for new treatments within five years."
Living with retinitis pigmentosa
Sisters Jane and Helen Walker, from Leeds, both have retinitis pigmentosa. They donated skin cells to the University, which helped the researchers make this genetic breakthrough.

Sisters Jane (left) and Helen Walker
Jane, 55, a retired school meals assistant, said: "We always used to struggle at school. It was hard to read and we couldn’t even see the blackboard, so we used to just muddle through. Mum and Dad only told us when we'd left school that we were visually impaired, they just wanted us to have a normal life as best we could.
"It's very difficult coping with the disease, but I manage. You can look at things in front of you but you can’t look down or to the sides at the same time.
"Martin McKibbin at St James’s Hospital got us involved in the research. I wanted to see if this study might help anyone else that shares our pain. It’s wonderful news that this research might soon be able to help other people."
Helen, 54, trains care workers and consults for a care home. She said: "I've got a tiny, tiny tunnel of vision now – it's like looking through a pinhole. Having no peripheral vision at all is really frightening. Anything on our periphery we just don’t see – it might be centimetres from our central vision.
"I get lots of injuries to my feet and to my head, because I'm very active. Broken toes and all kinds of things. In the dark we don’t have any sight at all.
"I became independent by using a guide dog called Tasmin. Tasmin's a life-saver but she's coming up to retirement age, and I’ve become very reliant on her. Believe me trying to navigate and negotiate streets, furniture, curbs, and particularly cars parked on pavements, is incredibly difficult with just a long white cane.
 Helen Walker with her guide dog Tasmin
Helen Walker with her guide dog Tasmin
"I went for some genetic counselling when I found out I had the disease, and I saw a doctor in Leeds. That was shocking, when I think about that appointment. She was talking to me about potentially becoming pregnant, and she was saying if it was determined that it was going to be a boy then you could consider termination because it would be a greater risk of him being blind. And I just walked out of the room, because I wouldn’t choose a life, if it was a boy or a girl.
"That was really difficult. The way she was speaking about it was horrible for me to contemplate. It was basically 'why would you want to have a blind child?', whereas I'd been one. It was horrible."
Helen brought up three step-children as her own.
"This research came at the right time and I was more than happy to do it. You've always got to have hope. You do it for other people, but there’s also a selfishness as well, because I want to know what it would be like to have more sight."
'Proof-of-concept'
Robert Holt, 57, is from Castleford and works for his local authority. He has retinitis pigmentosa and also donated skin cells to researchers at Leeds.
 Robert Holt with his granddaughter and partner
Robert Holt with his granddaughter and partner
"I've always had problems with my vision, I've always been short-sighted. My dad had the disease, and my auntie has it, but my earliest memories of it are probably not being able to see in the dark very well, which is one of the early indicators. And if you go from a light place to somewhere dark, that's what affects me most.
"This research is the proof-of-concept. With this disease affecting my family, I’m going to help however I can. We've always been supporters of the RP Fighting Blindness society. They're a charity which do fundraising, they give out money for research and helped fund this work.
"Any chance of working towards a treatment is fantastic. I mean you’re talking about a treatment for causes of blindness, which is amazing. Especially given that just a few years ago there was no hope.
"These trials have got to go ahead for them to try and make a bit of progress, and it looks like they've exceeded their expectations, which is brilliant. It may not help me, but future generations should be able to gain if a treatment is available. And if they do get a treatment at an early age, they could have normal sight for the rest of their life, which is fantastic."
International collaboration
Retinitis pigmentosa affects around 23,000 people in the UK and up to 2.5 million worldwide.
The research was conducted in collaboration with 38 researchers worldwide, including the Max Planck Institute in Göttingen, Germany, University of Durham, Harvard Medical School, State University of New York at Buffalo, King Abdulaziz University, Saudi Arabia, and the University of the West of England.
Tina Houlihan, Chief Executive of the charity Retina UK, said: "We are delighted that our support has enabled the group to publish these important findings in Nature Communications. We look forward to seeing the development of this work through our newly awarded grant, which will allow Professor Lako and the team to further understand the mechanisms underlying this type of RP and progress towards the targeted treatment strategies our community needs.”
Fight For Sight, the European Research Council, Retina UK and the Medical Research Council all helped fund the research.
Further information
For further information and to request interviews please email the University of Leeds press office at pressoffice@leeds.ac.uk
The paper, "Disrupted alternative splicing for genes implicated in splicing and ciliogenesis causes PRPF31 retinitis pigmentosa", is online here: https://www.nature.com/articles/s41467-018-06448-y
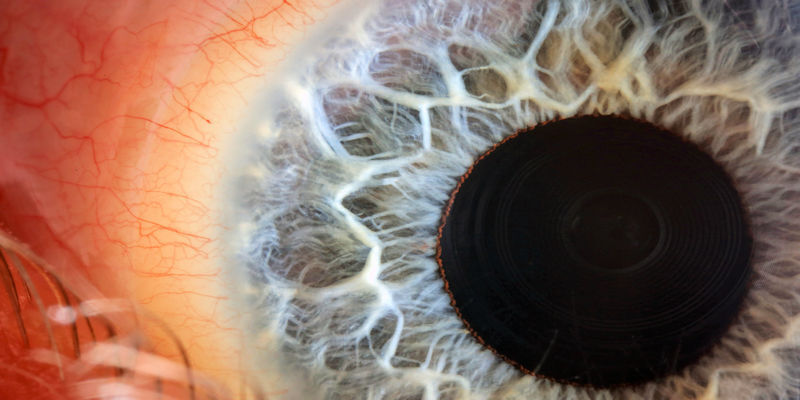
Main image: 'Human eye with blue iris', by Macroscopic Solutions.
This article was amended to update the name of charity RP Fighting Blindness to its new name Retina UK.