Medical imaging researchers have developed a new technology which can measure oxygen levels in tumours in real time, potentially paving the way for better targeted treatment of certain cancer cells.
The development is a major step towards the researchers’ ultimate goal of being able to identify which tumours are starved of oxygen, an important factor in deciding how effectively they can be treated by radiotherapy.
The study, a collaboration between the University of Leeds, the University of Manchester, the Institute of Cancer Research and University College London, has been published in the journal Radiotherapy and Oncology.
Funded mainly by the Medical Research Council, the breakthrough was achieved by the research team combining cutting-edge technologies, showing that an MRI scanner which also delivers radiotherapy – known as an MR-Linac – is able to measure the oxygen levels in tumours.
The University of Leeds’s Professor David Buckley, who co-authored the study, said: “It's very encouraging to see the results of this study, which is the latest output from a research collaboration between myself and colleagues in Manchester that started almost 20 years ago. The findings open up exciting new opportunities for developing this technology in the future.”
Despite this knowledge, patients with cancer do not get routine tests to evaluate tumour oxygen levels because no single test has been developed that is precise, accurate, cost effective and readily available.
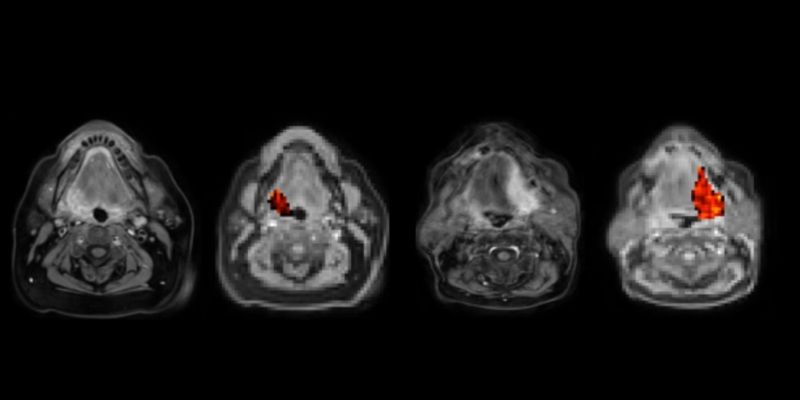
Patients with head and neck cancer in the study were successfully scanned on the MR-Linac machine at The Christie Hospital in Manchester and, for the first time, maps of oxygen levels were obtained. The technology is relevant to many cancers, not just head and neck cancer.
The patients first breathed room air through a mask and then pure oxygen to bathe the tumour with the gas.
Parts of the cancer that had good levels of oxygen responded differently to those that were oxygen depleted. The technique – called 'oxygen-enhanced MRI' – revealed which parts of the tumour were oxygen-starved and likely to be resistant to radiotherapy.
Lead author Professor James O’Connor is a clinician scientist at The University of Manchester, The Christie Hospital NHS Foundation Trust and The Institute of Cancer Research.
He said: “Though it’s clear more work needs to be done, we’re very excited about the potential this technology has to enable daily monitoring of tumour oxygen and we hope to be at a point soon when the technology will guide cancer doctors in how they can best deliver radiotherapy.
“This imaging lets us see inside tumours and helps us understand why some people with cancer need an extra boost to get effective treatment. This is an important step towards the goal of changing treatment based on imaging biology.”
First author Michael Dubec from The Christie and the University of Manchester said: “MR-Linac is an exciting technology that combines highly precise imaging and radiotherapy delivery that allows for real-time imaging.
“We are tremendously excited about what is the first application in humans of 'oxygen-enhanced MRI', developed as a result of a multi-disciplinary team working across the country which has exciting implications on patient outcomes.”
Further information
The paper 'First-in-Human Technique Translation of Oxygen-Enhanced MRI to an MR Linac System in Patients with Head and Neck Cancer' is published in the journal Radiotherapy and Oncology.
For more details, email Ben Johnson at b.johnson2@leeds.ac.uk.