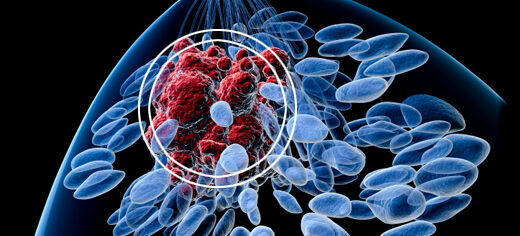
A drug commonly used in treating breast cancer could have far wider benefits, offering a new way of preventing cancers spreading through the body, according to a University of Leeds-led study.
The drug, geldanamycin, is well known for attacking a protein associated with the spread of breast cancer. However, a laboratory-based study found it also degraded a different protein that triggers blood vessel growth.
Stopping unwanted blood vessel growth is a key challenge in the battle against cancer, according to Dr Sreenivasan Ponnambalam, reader in human disease biology in the University of Leeds’ Faculty of Biological Sciences.
“This is potentially very significant because tumours secrete substances that stimulate blood vessels to develop around them, forming networks that supply nutrients and provide pathways for spread around the body,” Dr Ponnambalam said. “This is one of the big problems in cancer: how can we stop the tumour growing and spreading through these blood vessel networks?”
There are already other drugs available that try to stop this growth. One type tries to attack directly the membrane protein VEGFR2, which is essential for new blood vessel growth. However, that approach carries the risk of serious side-effects because proteins in the membrane walls of blood vessels do important work such as controlling blood pressure.
Geldanamycin offers a novel and potentially safer solution because it suppresses the protein indirectly.
The new study, based on experiments with human cells and different animal models, found that geldanamycin indirectly triggered the clearance of the VEGFR2 protein by activating a cellular quality-control system that breaks down many proteins.
That quality-control system already degrades VEGFR2 relatively slowly but the drug accelerates the process, preventing activation of the protein and inappropriate new blood vessel formation.
“With conventional treatments, we have been trying to deal with the situation after the switch has been thrown. What this drug does is destroy the key part of the switch before that switch is thrown,” Dr Ponnambalam said.
“Geldanamycin and chemical derivatives have been under intensive study in the laboratory and in clinical trials for the past 20 years. The cost to the NHS or patients could be relatively low compared to the expensive existing anti-cancer drugs, which are still under patent,” Dr Ponnambalam added.
The two-year study involved researchers in the University of Leeds and University College London. It was funded by The Wellcome Trust. The paper is published in the journal PLOS ONE.
Further information
Contact: University of Leeds Communications & Press Office: Tel +44 (0)113 343 4031, email pressoffice@leeds.ac.uk
The full paper: A.F Bruns N. Yuldasheva, A.M. Latham, Caroline Pellet-Many, L. Bao, P. Frankel, S.L. Stephen, G.J. Howell, S.B. Wheatcroft, M.T. Kearney, I.C. Zachary, S. Ponnambalam, “A heat-shock protein axis regulates VEGFR2 proteolysis, blood vessel development and repair.” PLOS ONE (2012)
The paper is available for download at http://dx.plos.org/10.1371/journal.pone.0048539%20 .